 The traditional physical examination is often significantly limited in the diagnosis of cardiopulmonary pathology. These diagnostic shortcomings are exaggerated in acutely ill ICU patients. Hand-carried ultrasounds (HCUs) are a new generation of portable ultrasound machines that are lightweight (6 to 10 lb), battery powered, and much less expensive (< $15,000) than the sophisticated “high-end” machines. Despite the fact that their initial introduction into clinical patient care was met with some criticism, the tremendous potential of HCUs to immediately provide diagnostic information at the bedside not assessable by the physical examination alone has been increasingly demonstrated and recognized in the last few years. These devices may facilitate the full clinical potential of ultrasound imaging in the ICU, with true portability, ease of use, and low cost. They are especially powerful when used as an adjunct to the physical examination.
The traditional physical examination is often significantly limited in the diagnosis of cardiopulmonary pathology. These diagnostic shortcomings are exaggerated in acutely ill ICU patients. Hand-carried ultrasounds (HCUs) are a new generation of portable ultrasound machines that are lightweight (6 to 10 lb), battery powered, and much less expensive (< $15,000) than the sophisticated “high-end” machines. Despite the fact that their initial introduction into clinical patient care was met with some criticism, the tremendous potential of HCUs to immediately provide diagnostic information at the bedside not assessable by the physical examination alone has been increasingly demonstrated and recognized in the last few years. These devices may facilitate the full clinical potential of ultrasound imaging in the ICU, with true portability, ease of use, and low cost. They are especially powerful when used as an adjunct to the physical examination.
An examination using HCU is usually “directed” toward a specific clinical question and is in general significantly shorter in duration (< 6 min in some studies) than one using traditional echocardiogra-phy. The disadvantage of such directed examinations with hand-carried devices are that they are not as comprehensive and can potentially miss some findings compared to traditional echocardio-graphic examinations. However, the HCU devices should not be compared with the yield or quality of the high-end machines. The HCU should be viewed more as an extension to the physical examina-tion. The accuracy of HCU is not simply one of whether the device produces good images. The factors used to define the accuracy of HCU include the capabilities of the device (imaging modes, accuracy of image) as well as the skill and training of the operator, the circumstances in which the examination is performed, the way it compares with physical examination, and the way it compares with standard echocardiography. Imaging modes and capabilities of currently available HCU machines vary, with color Doppler (true Doppler vs power Doppler), spectral Doppler, harmonics, and capacity to output video and image storage. In general, the accuracy of images created by these devices has shown good agreement when compared to standard echocardiographic machines with respect to two-dimensional findings. Technical limitations of the HCU are mainly due to their small screen (4 to 6 inches) and their limited color Doppler capabilities. Studies have shown HCU sensitivity of two-dimensional imaging for finding abnormal LV function to range from 76 to 96% with lower sensitivity for color Doppler assessment of valvular regurgitation (52 to 96%). Most studies comparing HCU with standard echocardiography were done in the inpatient ward or outpatient practice setting. A recent study done by Gorcsan et al investigated the utility of the HCU when specifically used as an extension of the physical examination on consultative cardiology rounds (n = 235). The HCU demonstrated an excellent close overall agreement (92 to 100%, r = 0.91 to 0.96) for estimation of EF, LV hypertrophy, regional wall motion abnormalities, and pericardial effusion (as assessed by two-dimensional imaging) when compared to an echocardiographic study using a full-size echocardiographic system. The “goal-directed” HCU study was performed in 150 cases and having interpreted > 300) if the goal is the performance and interpretation of a complete echocardio-graphic study as suggested by the American College of Cardiology and the American Heart Associa-tion. However, a lower degree of training is feasible when the goal is to perform a focused examination used as an extension to the physical examination. A focused examination in this context consists mostly in defining ventricular function and diagnosing a pericardial effusion. HCU studies performed by noncardiology medical personnel (medical students, residents, internists) have been demonstrated to be diagnostic in 75 to 90% of patients with a correct interpretation in > 70 to 80% of patients. Training in these studies consisted of 30 min to 40 h of didactic training with some supervised “hands-on” experience. It should be emphasized that the goal of using HCU in the ICU should not be to replace high-end machines but to provide diagnostic data not detected on physical examination. HCU should allow critical care physicians to diagnose certain cardiopulmonary pathologies more rapidly than with standard echocardiography (which are often performed with a variable delay after having been requested). Provided that physicians performing point-of-care examinations with the HCU have adequate training, have realistic expectations, and understand the limitations of the device, then the HCU has the potential to create a tremendous advantage for bedside assessment and treatment of the ICU patient.
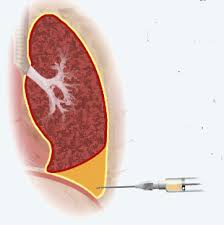 The value of HCU in the ICU extends beyond the cardiovascular examination in that it allows for the safe performance of bedside procedures that have traditionally been performed blindly. A HCU device will reduce complications associated with central venous cannulation and should be considered the standard of care when performing such hazardous procedures as thoracentesis in patients receiving mechanical ventilation. Equipping critical care physicians with HCUs and training them to perform point-of-care examinations will potentially translate into improved patient care. Although a benefit in terms of clinical outcomes remains to be demonstrated, the utility and impact of HCU at the bedside of critically ill patients can no longer be denied.
The value of HCU in the ICU extends beyond the cardiovascular examination in that it allows for the safe performance of bedside procedures that have traditionally been performed blindly. A HCU device will reduce complications associated with central venous cannulation and should be considered the standard of care when performing such hazardous procedures as thoracentesis in patients receiving mechanical ventilation. Equipping critical care physicians with HCUs and training them to perform point-of-care examinations will potentially translate into improved patient care. Although a benefit in terms of clinical outcomes remains to be demonstrated, the utility and impact of HCU at the bedside of critically ill patients can no longer be denied.
Performance of Bedside Ultrasonography by the Intensivist
It is usually not feasible to have a cardiologist or sonographer available on immediate call on a 24-h basis to perform bedside ultrasonographic examinations in the ICU. The value of immediate bedside echocardiography for aiding in diagnosis and management of acute hemodynamic disturbances has been well demonstrated in both the ICU and the emergency department. It is recognized that ultrasound technologies are not exclusive to the radiologist or cardiologist. Appropriately trained emergency department physicians, surgeons, anesthesiologists, and intensive care specialists have been using ultrasound devices with great success. Anesthesiologists were instrumental in many of the pioneering studies of TEE in the operating room and ICU. Successful performance of bedside echocardiography by noncardiologist intensivists has also been well demonstrated in the litera-ture. Benjamin et al showed that a limited TEE examination performed and interpreted by intensivists (after training under the supervision of two cardiologists) is feasible and provides rapid, accurate diagnostic information that can have a dramatic impact on the treatment of critically ill patients. The safety and utility of performance of bedside ultrasound by the intensivist for various other purposes in the ICU (central venous cannula-tion, thoracentesis, paracentesis) have also been well demonstrated. With the increasing popularity of HCU devices, there is controversy “in some circles” regarding both the advisability and use of noncomprehensive goal-directed examinations performed by noncardiologists or nonradiologists.
 Studies with these portable devices have demonstrated that they can provide important clinical information (see the previous section on HCU) but that even in highly skilled hands they may provide suboptimal imaging or diagnostic capabilities in the ICU setting. The era of a technology-extended physical examination appears to have arrived, and there appears to be a role for a user-specific, focused ultrasound examinations. However, adequate training is essential, and this must be individualized and tailored to the specific needs and applications of the user. With expert back-up, “focused” bedside ultrasonography by in-tensivists is not only feasible but can be done safely and rapidly and yield information pertinent to the management of critically ill patients. However, inappropriate interpretation or application of data gained by a poorly skilled user may have adverse conse-quences. To avoid misusing this technology, adequate training is essential.
Studies with these portable devices have demonstrated that they can provide important clinical information (see the previous section on HCU) but that even in highly skilled hands they may provide suboptimal imaging or diagnostic capabilities in the ICU setting. The era of a technology-extended physical examination appears to have arrived, and there appears to be a role for a user-specific, focused ultrasound examinations. However, adequate training is essential, and this must be individualized and tailored to the specific needs and applications of the user. With expert back-up, “focused” bedside ultrasonography by in-tensivists is not only feasible but can be done safely and rapidly and yield information pertinent to the management of critically ill patients. However, inappropriate interpretation or application of data gained by a poorly skilled user may have adverse conse-quences. To avoid misusing this technology, adequate training is essential.
General guidelines in training for both TTE and TEE have been developed by the American Society of Echocardiography in association with the American Heart Association and the American College of Cardiology. Since 1996, the American Society of Anesthesiologists and Society of Cardiovascular Anesthesiologist have developed practice guidelines for perioperative TEE. The importance of adequate training and subsequent maintenance of competence cannot be overemphasized, as inappropriate use or misapplication could potentially temper the acceptance of bedside ultrasound by the intensivist. Training of intensivists and emergency department physicians in performance of emergency bedside ultrasound should provide rapid answers to clinical questions that may profoundly affect medical and surgical management decisions. Training in echocardiography and general ultrasonography should be incorporated in the critical care fellowship with special emphasis on TEE as part of the training program.^ It is hoped that critical care and echocar-diographic societies will, in the near future, credential such additional training.